Calculous prostatitis– a complication of chronic inflammation of the prostate gland, characterized by the formation of stones in the acini or excretory ducts of the gland. Calculous prostatitis is accompanied by increased urination, dull aching pain in the lower abdomen and perineum, erectile dysfunction, the presence of blood in the seminal fluid, and prostatorrhea. Calculous prostatitis can be diagnosed using a digital examination of the prostate, ultrasound of the prostate gland, survey urography, and laboratory examination. Conservative therapy for calculous prostatitis is carried out with the help of medications, herbal medicine, and physiotherapy; If these measures are ineffective, stone destruction with a low-intensity laser or surgical removal is indicated.
General information
Calculous prostatitis is a form of chronic prostatitis, accompanied by the formation of stones (prostatoliths). Calculous prostatitis is the most common complication of a long-term inflammatory process in the prostate gland, which specialists in the field of urology and andrology have to deal with. During preventive ultrasound examination, prostate stones are detected in 8. 4% of men of various ages. The first age peak in the incidence of calculous prostatitis occurs at 30-39 years of age and is due to an increase in cases of chronic prostatitis caused by STDs (chlamydia, trichomoniasis, gonorrhea, ureaplasmosis, mycoplasmosis, etc. ). In men 40-59 years old, calculous prostatitis, as a rule, develops against the background of prostate adenoma, and in patients over 60 years old it is associated with a decline in sexual function.
Causes of calculous prostatitis
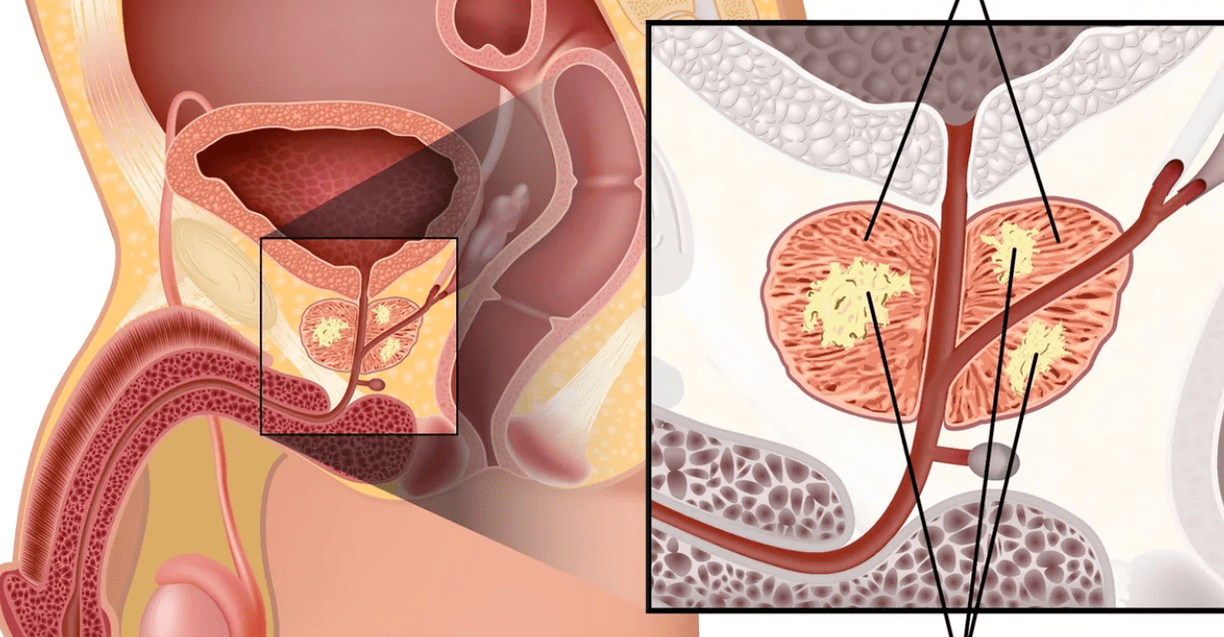
Depending on the cause of formation, prostate stones can be true (primary) or false (secondary). Primary stones initially form directly in the acini and ducts of the gland, secondary stones migrate into the prostate from the upper urinary tract (kidneys, bladder or urethra) if the patient has urolithiasis.
The development of calculous prostatitis is caused by congestive and inflammatory changes in the prostate gland. Impaired emptying of the prostatic glands is caused by BPH, irregularity or lack of sexual activity, and a sedentary lifestyle. Against this background, the addition of a sluggish infection of the genitourinary tract leads to obstruction of the prostate ducts and a change in the nature of the prostate secretion. In turn, prostate stones also support a chronic inflammatory process and stagnation of secretions in the prostate.
In addition to stagnation and inflammatory phenomena, urethro-prostatic reflux plays an important role in the development of calculous prostatitis - the pathological reflux of a small amount of urine from the urethra into the prostate ducts during urination. At the same time, the salts contained in the urine crystallize, thicken and, over time, turn into stones. The causes of urethro-prostatic reflux can be urethral strictures, trauma to the urethra, atony of the prostate and seminal tubercle, previous transurethral resection of the prostate gland, etc.
The morphological core for prostate calculi is amyloid bodies and desquamated epithelium, which are gradually "overgrown" with phosphate and calcareous salts. Prostate stones lie in cystically distended acini (lobules) or in the excretory ducts. Prostatoliths are yellowish in color, spherical in shape, and vary in size (on average from 2. 5 to 4 mm); may be single or multiple. In terms of their chemical composition, prostate stones are identical to bladder stones. With calculous prostatitis, oxalate, phosphate and urate stones are most often formed.
Symptoms of calculous prostatitis
The clinical manifestations of calculous prostatitis generally resemble the course of chronic inflammation of the prostate. The leading symptom in the clinic of calculous prostatitis is pain. The pain is dull, aching in nature; localized in the perineum, scrotum, above the pubis, sacrum or coccyx. Exacerbation of painful attacks may be associated with defecation, sexual intercourse, physical activity, prolonged sitting on a hard surface, prolonged walking or bumpy driving. Calculous prostatitis is accompanied by frequent urination, sometimes by complete urinary retention; hematuria, prostatorrhea (leakage of prostate secretions), hemospermia. Characterized by decreased libido, weak erection, impaired ejaculation, and painful ejaculation.
Endogenous prostate stones can remain in the prostate gland for a long time without symptoms. However, a long course of chronic inflammation and associated calculous prostatitis can lead to the formation of a prostate abscess, the development of vesiculitis, atrophy and sclerosis of the glandular tissue.
Diagnosis of calculous prostatitis
To establish a diagnosis of calculous prostatitis, a consultation with a urologist (andrologist), an assessment of existing complaints, and a physical and instrumental examination of the patient are required. When performing a rectal digital examination of the prostate, the lumpy surface of the stones and a kind of crepitus are determined by palpation. Using transrectal ultrasound of the prostate gland, stones are detected as hyperechoic formations with a clear acoustic track; their location, quantity, size and structure are clarified. Sometimes survey urography, CT and MRI of the prostate are used to detect prostatoliths. Exogenous stones are diagnosed by pyelography, cystography and urethrography.
An instrumental examination of a patient with calculous prostatitis is complemented by laboratory diagnostics: examination of prostate secretions, bacteriological culture of urethral discharge and urine, PCR examination of scrapings for sexually transmitted infections, biochemical analysis of blood and urine, determination of the level of prostate-specific antigen, biochemistry of sperm, culture of ejaculate, etc.
When conducting an examination, calculous prostatitis is differentiated from prostate adenoma, tuberculosis and prostate cancer, chronic bacterial and abacterial prostatitis. In calculous prostatitis not associated with prostate adenoma, the volume of the prostate gland and PSA level remain normal.
Treatment of calculous prostatitis
Uncomplicated stones in combination with chronic inflammation of the prostate gland require conservative anti-inflammatory therapy. Treatment of calculous prostatitis includes antibiotic therapy, non-steroidal anti-inflammatory drugs, herbal medicine, physiotherapeutic procedures (magnetic therapy, ultrasound therapy, electrophoresis). In recent years, low-intensity laser has been successfully used to non-invasively destroy prostate stones. Prostate massage for patients with calculous prostatitis is strictly contraindicated.
Surgical treatment of calculous prostatitis is usually required in the case of a complicated course of the disease, its combination with prostate adenoma. When a prostate abscess forms, the abscess is opened, and along with the outflow of pus, the passage of stones is also noted. Sometimes mobile exogenous stones can be instrumentally pushed into the bladder and subjected to lithotripsy. Removal of fixed stones of large sizes is carried out in the process of perineal or suprapubic section. When calculous prostatitis is combined with BPH, the optimal method of surgical treatment is adenomectomy, TUR of the prostate, prostatectomy.
Forecast and prevention of calculous prostatitis
In most cases, the prognosis for conservative and surgical treatment of calculous prostatitis is favorable. Long-term non-healing urinary fistulas can be a complication of perineal removal of prostate stones. In the absence of treatment, the outcome of calculous prostatitis is abscess formation and sclerosis of the prostate gland, urinary incontinence, impotence, and male infertility.
The most effective measure to prevent stone formation in the prostate gland is to contact a specialist when the first signs of prostatitis occur. An important role belongs to the prevention of STIs, elimination of predisposing factors (urethro-prostatic reflux, metabolic disorders), age-appropriate physical and sexual activity. Preventive visits to a urologist and timely treatment of urolithiasis will help to avoid the development of calculous prostatitis.






























